Personalized medicine, also known as precision medicine, represents a groundbreaking approach to healthcare that tailors medical treatment and interventions to individual characteristics, including genetic makeup, molecular profiles, lifestyle factors, and environmental influences. By leveraging advanced technologies, such as genomics, proteomics, and bioinformatics, personalized medicine aims to optimize therapeutic outcomes, minimize adverse effects, and improve patient satisfaction. In this comprehensive exploration, we delve into the transformative potential of personalized medicine, examining its principles, applications, challenges, and future directions.
 Principles of Personalized Medicine: From One-Size-Fits-All to Targeted Therapies
Principles of Personalized Medicine: From One-Size-Fits-All to Targeted Therapies
Traditional approaches to medical treatment often rely on a one-size-fits-all paradigm, where patients with similar diagnoses receive standardized treatments based on population-level guidelines and protocols. However, this approach fails to account for the inherent variability among individuals, leading to variability in treatment response, efficacy, and safety. Personalized medicine seeks to address this limitation by embracing the following principles:
Genomic Medicine: Genomic medicine focuses on understanding how variations in an individual’s genetic makeup influence disease risk, drug metabolism, and treatment response. Advances in DNA sequencing technologies, such as next-generation sequencing (NGS), enable comprehensive analysis of an individual’s genome, identifying genetic variants associated with disease susceptibility and treatment outcomes.
Precision Diagnostics: Precision diagnostics leverage molecular profiling techniques, such as gene expression analysis, proteomics, and metabolomics, to characterize the molecular signatures of diseases and guide targeted interventions. By identifying biomarkers and molecular targets specific to an individual’s condition, precision diagnostics enable more accurate diagnosis, prognosis, and treatment selection.
Individualized Treatment Plans: Personalized medicine tailors treatment plans and interventions to each patient’s unique characteristics, preferences, and needs. This may involve selecting medications based on genetic markers, adjusting dosages to account for variations in drug metabolism, or integrating lifestyle modifications and behavioral interventions to optimize therapeutic outcomes.
 Applications of Personalized Medicine: From Oncology to Preventive Health
Applications of Personalized Medicine: From Oncology to Preventive Health
Personalized medicine has diverse applications across various medical specialties and disease areas, offering new insights into disease pathogenesis, treatment response, and patient management. Key applications include:
Oncology: Personalized medicine has revolutionized cancer care by enabling the identification of molecular alterations driving tumor growth and progression. Targeted therapies, such as tyrosine kinase inhibitors and monoclonal antibodies, selectively target cancer cells harboring specific genetic mutations or molecular abnormalities, leading to improved treatment response rates and survival outcomes.
Pharmacogenomics: Pharmacogenomics studies how genetic variations influence an individual’s response to medications, including drug efficacy, toxicity, and adverse drug reactions (ADRs). By analyzing genetic markers associated with drug metabolism, pharmacodynamics, and drug interactions, pharmacogenomic testing informs personalized prescribing decisions, optimizing medication selection and dosing to maximize therapeutic benefit and minimize harm.
Preventive Health: Personalized medicine extends beyond the realm of disease treatment to encompass preventive health and wellness strategies. Genetic risk assessments, lifestyle interventions, and precision nutrition programs empower individuals to proactively manage their health, reduce disease risk, and optimize longevity.
 Challenges and Considerations in Personalized Medicine Implementation
Challenges and Considerations in Personalized Medicine Implementation
Despite its promise, personalized medicine faces several challenges and considerations that must be addressed to realize its full potential and ensure equitable access for all patients. Key challenges include:
Data Integration and Interoperability: Personalized medicine relies on the integration of diverse datasets, including genomic data, clinical records, and environmental factors, to generate actionable insights. However, data silos, interoperability issues, and privacy concerns can hinder data sharing and integration, limiting the utility of personalized medicine approaches in clinical practice.
Cost and Accessibility: The high cost of genomic testing, molecular diagnostics, and targeted therapies may pose barriers to widespread adoption and accessibility of personalized medicine. Socioeconomic disparities, insurance coverage limitations, and reimbursement challenges can exacerbate inequities in access to personalized healthcare services, particularly among underserved populations.
Ethical and Regulatory Frameworks: Personalized medicine raises ethical and regulatory considerations related to patient privacy, informed consent, data ownership, and equity in healthcare delivery. Safeguarding patient rights, ensuring transparency in data use, and promoting responsible innovation are essential for building public trust and regulatory confidence in personalized medicine approaches.
Future Directions: Innovations and Opportunities in Personalized Medicine
As personalized medicine continues to evolve, several emerging trends and innovations hold promise for advancing the field and addressing existing challenges. Key areas of focus include:
Artificial Intelligence and Machine Learning: AI-driven algorithms and machine learning models are enhancing personalized medicine approaches with advanced capabilities for data analysis, pattern recognition, and predictive modeling. AI-powered decision support systems, clinical decision algorithms, and predictive analytics tools enable more precise diagnosis, treatment planning, and patient stratification in personalized medicine.
Multi-Omics Integration: Multi-omics approaches integrate data from genomics, transcriptomics, proteomics, and metabolomics to provide a comprehensive understanding of disease mechanisms and treatment responses. By combining multi-dimensional molecular data with clinical information, multi-omics analyses enable more accurate disease classification, biomarker discovery, and therapeutic target identification in personalized medicine.
How To Prevent Cavities Naturally: EFFECTIVE STRATEGIES [2024]
NEW: Cosmetic Dentistry Insurance, What’s In and What’s Out, Important background Information[2024]
Patient-Centered Technologies: Patient-centered technologies, such as mobile health apps, wearable sensors, and digital health platforms, empower individuals to actively participate in their healthcare journey and engage with personalized interventions. Remote monitoring, self-tracking, and real-time feedback mechanisms enable patients to monitor their health status, track treatment progress, and communicate with healthcare providers in real-time, promoting shared decision-making and patient empowerment.
Personalized medicine represents a paradigm shift in healthcare delivery, offering a transformative approach that prioritizes individualized care, targeted interventions, and precision diagnostics. By harnessing the power of genomic insights, molecular profiling, and advanced technologies, personalized medicine has the potential to revolutionize disease management, improve treatment outcomes, and enhance the quality of life for patients worldwide. As we navigate the complexities of personalized medicine implementation, it is essential to address technological, ethical, and regulatory challenges while embracing innovations that advance the field and promote equitable access to personalized healthcare for all individuals. With continued innovation, collaboration, and commitment to patient-centered care, personalized medicine holds the promise of ushering in a new era of healthcare that is truly tailored to the needs and preferences of each individual.
The Luxury Toothpaste Trend: Worth the Price Tag? (2024 INSIGHTS)
Hidden Costs of Oral Health Neglect and How to Avoid Them (2024)
 Principles of Personalized Medicine: From One-Size-Fits-All to Targeted Therapies
Principles of Personalized Medicine: From One-Size-Fits-All to Targeted Therapies Applications of Personalized Medicine: From Oncology to Preventive Health
Applications of Personalized Medicine: From Oncology to Preventive Health In an era defined by technological innovation and interconnectedness, telemedicine has emerged as a transformative force in healthcare delivery, offering new avenues for remote consultation, diagnosis, treatment, and monitoring. With advancements in digital communication, mobile technology, and virtual care platforms, telemedicine has the potential to expand access to healthcare services, improve patient outcomes, and enhance the efficiency of healthcare delivery systems. In this comprehensive exploration, we delve into the multifaceted realm of telemedicine, examining its evolution, applications, benefits, challenges, and future directions.
In an era defined by technological innovation and interconnectedness, telemedicine has emerged as a transformative force in healthcare delivery, offering new avenues for remote consultation, diagnosis, treatment, and monitoring. With advancements in digital communication, mobile technology, and virtual care platforms, telemedicine has the potential to expand access to healthcare services, improve patient outcomes, and enhance the efficiency of healthcare delivery systems. In this comprehensive exploration, we delve into the multifaceted realm of telemedicine, examining its evolution, applications, benefits, challenges, and future directions. Applications of Telemedicine in Healthcare
Applications of Telemedicine in Healthcare
 Future Directions: Innovations and Opportunities in Telemedicine
Future Directions: Innovations and Opportunities in Telemedicine Unleashing the Power of Data: AI Applications in Healthcare
Unleashing the Power of Data: AI Applications in Healthcare Challenges and Opportunities: Navigating the AI Landscape in Healthcare
Challenges and Opportunities: Navigating the AI Landscape in Healthcare Future Directions: Innovations and Challenges on the Horizon
Future Directions: Innovations and Challenges on the Horizon In recent years, the United States has been gripped by a devastating epidemic of opioid misuse, addiction, and overdose deaths. This complex public health crisis has exacted a profound toll on individuals, families, and communities across the nation, highlighting the urgent need for comprehensive strategies to combat opioid misuse and prevent further harm. In this comprehensive examination, we delve into the multifaceted dimensions of the opioid epidemic, exploring its origins, impacts, and potential solutions to mitigate its devastating effects.
In recent years, the United States has been gripped by a devastating epidemic of opioid misuse, addiction, and overdose deaths. This complex public health crisis has exacted a profound toll on individuals, families, and communities across the nation, highlighting the urgent need for comprehensive strategies to combat opioid misuse and prevent further harm. In this comprehensive examination, we delve into the multifaceted dimensions of the opioid epidemic, exploring its origins, impacts, and potential solutions to mitigate its devastating effects.
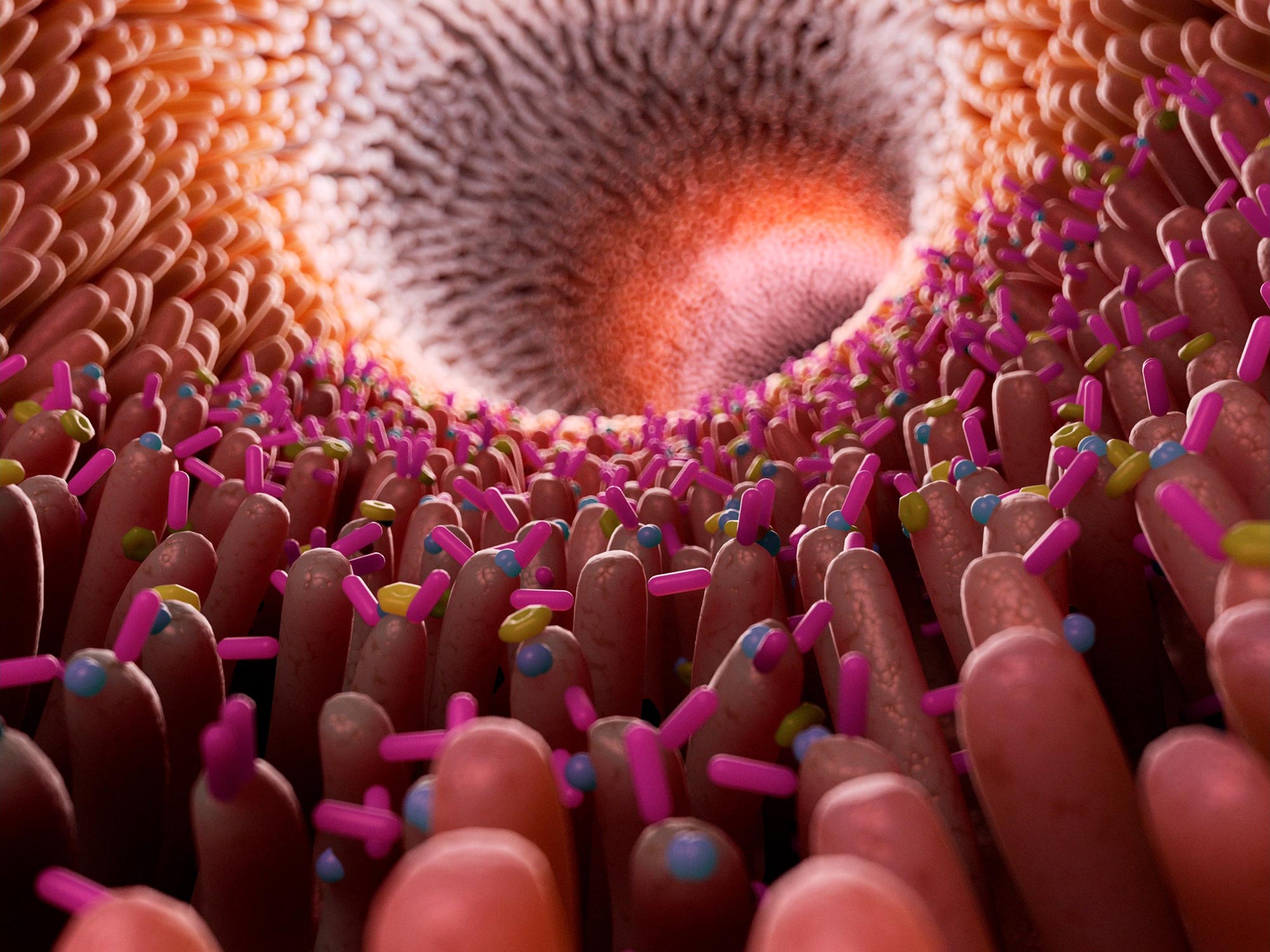 In the intricate ecosystem of the human body, trillions of microorganisms coexist in a delicate balance, shaping health, immunity, and disease. This bustling community of bacteria, viruses, fungi, and other microbes—collectively known as the microbiome—plays a vital role in various physiological processes, from digestion and metabolism to immune regulation and neurological function. In this comprehensive exploration, we delve into the captivating world of the microbiome, unraveling its mysteries, probing its significance, and exploring its potential implications for human health and wellness.
In the intricate ecosystem of the human body, trillions of microorganisms coexist in a delicate balance, shaping health, immunity, and disease. This bustling community of bacteria, viruses, fungi, and other microbes—collectively known as the microbiome—plays a vital role in various physiological processes, from digestion and metabolism to immune regulation and neurological function. In this comprehensive exploration, we delve into the captivating world of the microbiome, unraveling its mysteries, probing its significance, and exploring its potential implications for human health and wellness.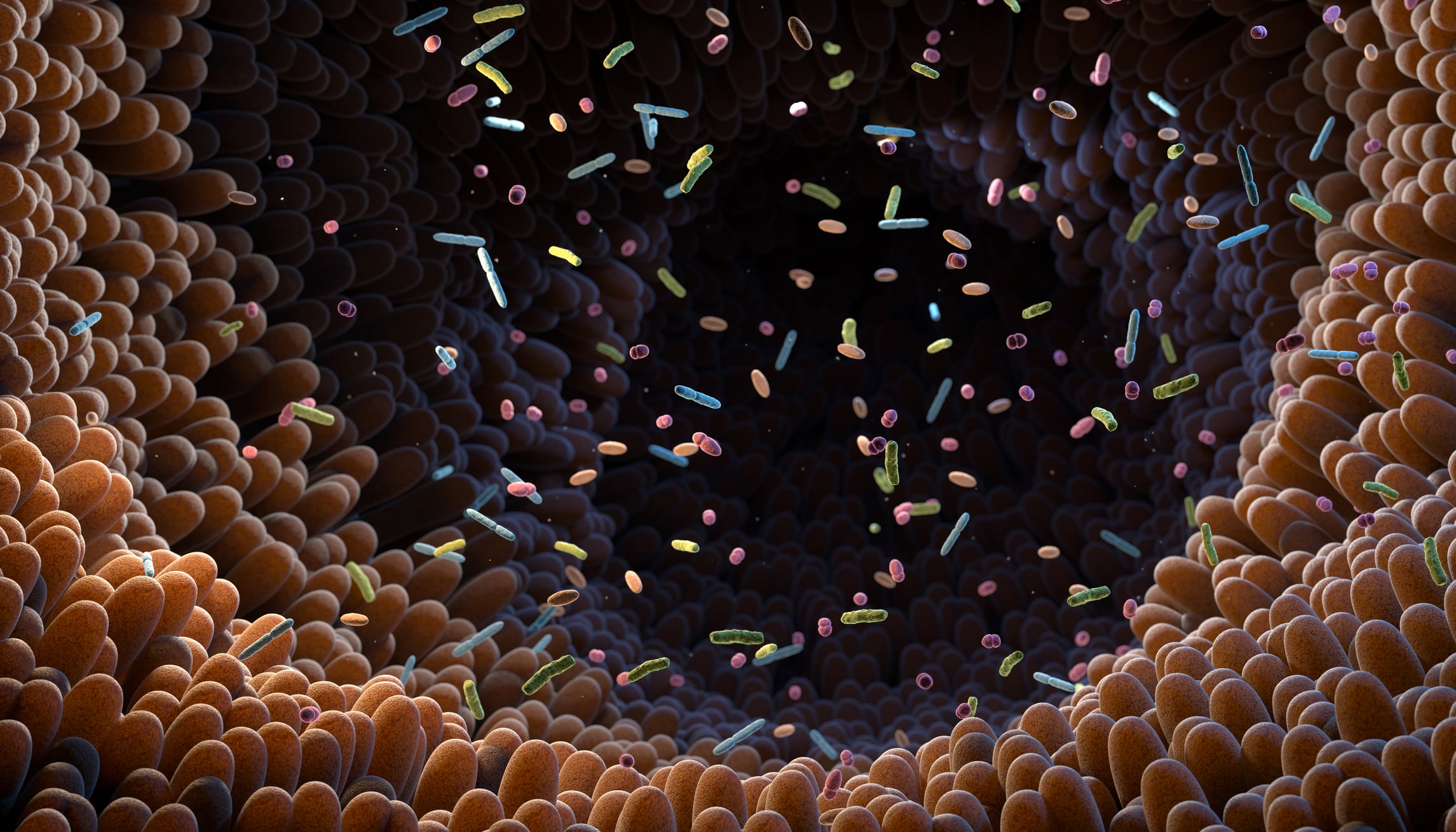 The Gut-Brain Axis: Exploring the Mind-Gut Connection
The Gut-Brain Axis: Exploring the Mind-Gut Connection Ethical and Social Implications: Navigating the Microbial Frontier
Ethical and Social Implications: Navigating the Microbial Frontier In the ever-evolving landscape of medical science, breakthroughs and innovations continuously redefine our understanding of health, disease, and the human body. From cutting-edge technologies to groundbreaking treatments, the field of medicine is a dynamic realm where discovery knows no bounds. In this comprehensive overview, we delve into a myriad of medical topics, exploring recent advancements, emerging trends, and the potential impact on healthcare and society at large.
In the ever-evolving landscape of medical science, breakthroughs and innovations continuously redefine our understanding of health, disease, and the human body. From cutting-edge technologies to groundbreaking treatments, the field of medicine is a dynamic realm where discovery knows no bounds. In this comprehensive overview, we delve into a myriad of medical topics, exploring recent advancements, emerging trends, and the potential impact on healthcare and society at large.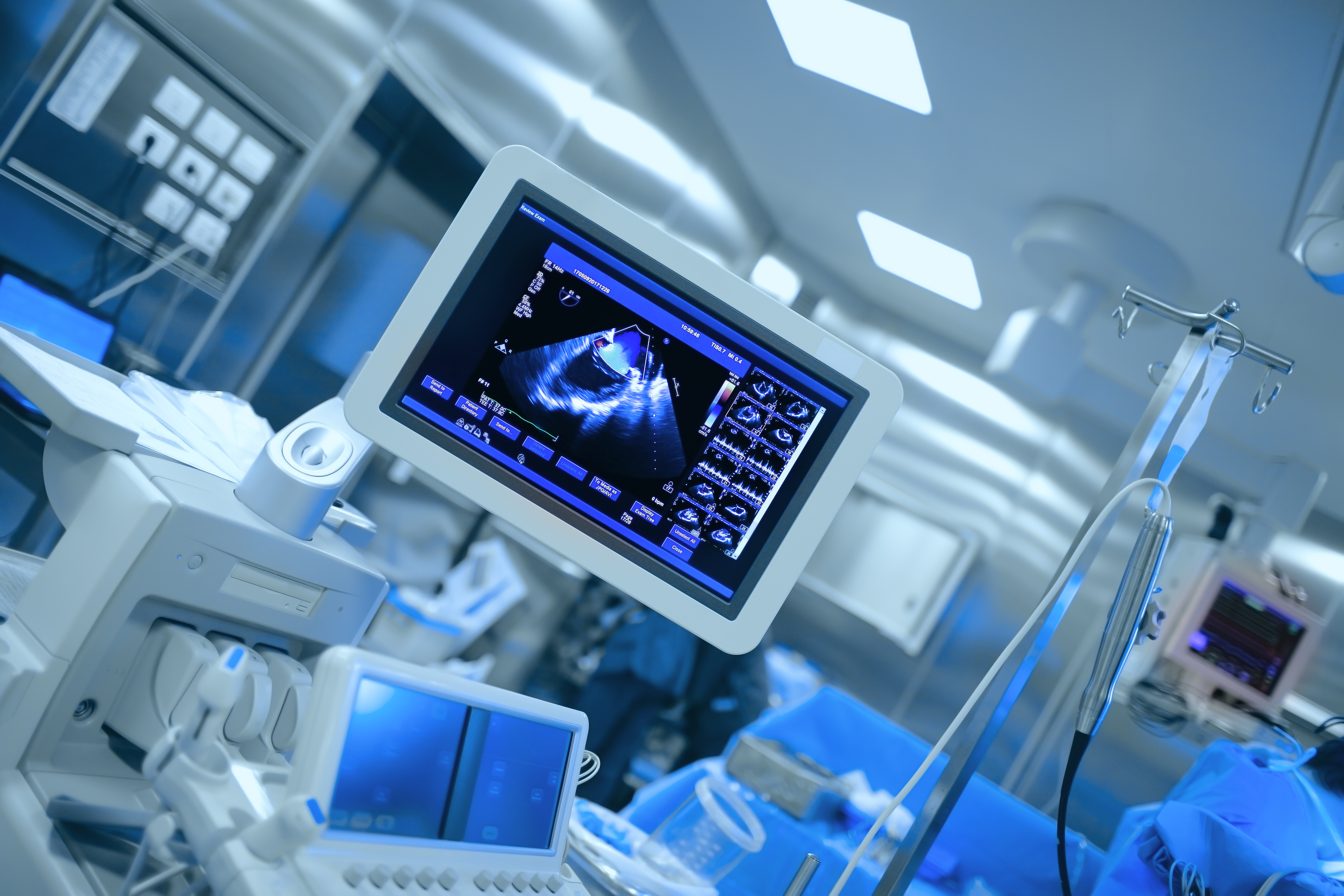 Artificial Intelligence in Healthcare: Revolutionizing Diagnosis and Treatment
Artificial Intelligence in Healthcare: Revolutionizing Diagnosis and Treatment Telemedicine: Transforming Healthcare Delivery
Telemedicine: Transforming Healthcare Delivery In the vast expanse of the universe, few phenomena capture the imagination and curiosity of humanity quite like black holes. These enigmatic cosmic entities, shrouded in mystery and intrigue, defy conventional understanding and beckon us to explore the depths of space-time. From their formation to their profound influence on the fabric of the cosmos, black holes remain one of the most captivating subjects in astrophysics. In this comprehensive exploration, we embark on a journey to unravel the secrets of black holes, delving into their origins, characteristics, and significance in the cosmic tapestry.
In the vast expanse of the universe, few phenomena capture the imagination and curiosity of humanity quite like black holes. These enigmatic cosmic entities, shrouded in mystery and intrigue, defy conventional understanding and beckon us to explore the depths of space-time. From their formation to their profound influence on the fabric of the cosmos, black holes remain one of the most captivating subjects in astrophysics. In this comprehensive exploration, we embark on a journey to unravel the secrets of black holes, delving into their origins, characteristics, and significance in the cosmic tapestry. Formation and Evolution: Cosmic Birth and Death
Formation and Evolution: Cosmic Birth and Death Unveiling the Mysteries: Probing Black Hole Characteristics
Unveiling the Mysteries: Probing Black Hole Characteristics Beyond the Event Horizon: Exploring Black Hole Phenomena
Beyond the Event Horizon: Exploring Black Hole Phenomena Black Holes: Cosmic Architects and Cosmic Destroyers
Black Holes: Cosmic Architects and Cosmic Destroyers The Paradox of Black Holes: Unanswered Questions and Future Frontiers
The Paradox of Black Holes: Unanswered Questions and Future Frontiers The Cosmic Odyssey Continues: Charting New Horizons
The Cosmic Odyssey Continues: Charting New Horizons In the realm of dentistry, braces stand as both a marvel of modern orthodontics and a potential source of dread for many individuals. These orthodontic appliances, consisting of wires, brackets, and bands, are designed to correct misaligned teeth and jaws, offering not only aesthetic benefits but also functional improvements in bite alignment and overall oral health. However, despite their numerous advantages, braces can also evoke apprehension due to discomfort, maintenance requirements, and social stigmas. In this comprehensive guide, we delve into the world of braces, exploring what they are, why they are needed, the challenges they pose, and whether they are truly indispensable in achieving optimal dental health.
In the realm of dentistry, braces stand as both a marvel of modern orthodontics and a potential source of dread for many individuals. These orthodontic appliances, consisting of wires, brackets, and bands, are designed to correct misaligned teeth and jaws, offering not only aesthetic benefits but also functional improvements in bite alignment and overall oral health. However, despite their numerous advantages, braces can also evoke apprehension due to discomfort, maintenance requirements, and social stigmas. In this comprehensive guide, we delve into the world of braces, exploring what they are, why they are needed, the challenges they pose, and whether they are truly indispensable in achieving optimal dental health. Why You Need Braces
Why You Need Braces Are Braces Truly Necessary?
Are Braces Truly Necessary? # How to Choose the Best Health Insurance Plan for You and Your Family
# How to Choose the Best Health Insurance Plan for You and Your Family Types of health insurance plans
Types of health insurance plans There are many resources and tools that can help you in choosing the best health insurance plan for you and your family. Some of the main resources and tools are:
There are many resources and tools that can help you in choosing the best health insurance plan for you and your family. Some of the main resources and tools are: # Research and Data on Insurance: How They Shape the Industry and Society
# Research and Data on Insurance: How They Shape the Industry and Society Types of research and data on insurance
Types of research and data on insurance